The State of Healthcare Workforce Shortages: Challenges, Causes, and Solutions

The challenge that has haunted healthcare executives, exhausted our workforce, driven policy changes, and sparked numerous studies and analyses? You guessed it—shortages. Healthcare shortages have plagued our system even before the pandemic, and they’ve skyrocketed since. By 2022, an estimated 100,000 RNs left the workforce due to stress, burnout, or retirement, largely driven by pandemic pressures.
The fallout from these shortages? A devastating clinician exodus fueled by burnout and exhaustion. Workers who have stayed are now burned out, exhausted, and dissatisfied. Healthcare facilities are overwhelmingly understaffed and under budget.
What’s worse, projections from several reputable sources indicate that shortages are a trend that’s set to continue, but maybe not necessarily in the way we once thought.
Healthcare jobs are set to outpace all other industries in job growth over the next decade, with an expected 1.6 million new jobs by 2033—24% of all new jobs in the economy. Though shortages are expected to peak, especially with an aging population requiring more care, there’s a glimmer of hope.
In this article, we’ll explore the latest reports, research, and data on healthcare workforce shortages, including how projections have shifted from previous estimates, offering hope for the future. In an era of dissatisfied workers and poor working conditions, it’s crucial to not only examine the numbers but also the steps being taken to combat shortages through human-centered and technology-driven approaches. We’ll cover the data, regional projections, impacts, and strategies being implemented to address healthcare labor shortages.
What Are Healthcare Workforce Shortages?
Shortages in healthcare refer to the gap between the decreasing supply of healthcare workers and the increasing demand for patient care. This means there are not enough qualified professionals with the right skills to provide medical attention to a growing population in need.
A deficit in these essential workers has several severe consequences for everyone. For the patient seeking care, they may not be able to be seen. For those able to be taken care of, the quality of care may be compromised due to workers spreading themselves thin amongst several patients. For healthcare employees, this means further strain in a time where workers are overworked and burned out due to little assistance and necessary staff levels.
Causes of Workforce Shortages
1. Aging Population
An aging population plays into the healthcare shortage problem in two significant ways. First, a large demographic is reaching an age where chronic illnesses are more common, leading to a greater need for medical attention and increasing demand. The second dilemma is the aging healthcare workforce itself, as many healthcare professionals are preparing for their own retirement, resulting in a loss of valuable skills and widening the gap between supply and demand.
Let’s look at some of the numbers from the Census Bureau to better understand the situation. According to the most recent census in 2023, there were 55.8 million Americans aged 65 or older. This is expected to grow exponentially to 82 million by 2050—a 47% increase.
With Americans living longer than ever before, the likelihood of chronic illnesses rises, which means even greater care will be needed. The American Hospital Association’s 2025 Workforce Scan emphasizes the strain this demographic shift will place on the workforce. They estimate that instead of the current ratio of four workers per senior, there will be only 2.9 workers per senior in the next five years.
2. Aging Workforce
A large subset of the population reaching 65 years or older not only means greater care demands that need to be met, but it also implies that healthcare professionals nearing retirement will exit the workforce, further shrinking an already struggling labor pool.
The pandemic accelerated early retirements and prompted many professionals, especially nurses, to leave the workforce all together. The 2022 National Nursing Workforce Survey predicted that more than one-quarter of nurses will leave or retire by 2027. Additionally, the American Medical Association (AMA) estimates that in the next five years, 35% of the physician workforce will reach retirement. The AMA’s 2024 report further points out that physicians who are currently 65 years or older make up 20% of the clinical physician workforce, while those aged 55-64 comprise 22%. That’s nearly 44% of the physician workforce either already retiring or nearing retirement, resulting in a devastating hit to physician supply.
3. Education
One often overlooked factor contributing to workforce shortages is education, especially when we consider the shortage of educators in the healthcare field. This is incredibly impactful, as universities become limited in how many students they can enroll due to lack of qualified faculty. This, in turn, restricts the number of graduates entering the healthcare profession.
This can be particularly felt in nursing, where US nursing schools turned away 65,766 qualified applications in 2023. While faculty shortages were a primary factor, other issues such as limited resources, a lack of clinical sites, and budget constraints also played a role. According to the American Association of Colleges of Nursing (AACN), the nurse faculty vacancy rate stood at 7.8% in 2023, with 1,977 full-time faculty vacancies across 922 universities.
The nurse shortage itself is driven by several factors, including:
- Lucrative compensation outside the education setting, which draws experienced nurses to higher-paying clinical roles.
- A limited pool of educators with advanced degrees, such as Master’s or Doctoral qualifications.
- Increasing retirements among the existing educator workforce.
4. Burnout and Job Dissatisfaction
It’s a force that’s persisted and exhausted our healthcare teams. Burnout. In a corrosive cycle, burnout is fueled by turnover and shortages, where shortages lead to worker burnout, leading to increased turnover, further worsening shortages and burnout. It can be characterized by diminished professional satisfaction, strained work-life balance, and a sense of overwhelming fatigue.
Though shortages play a major role in contributing to worker stress and burnout, the weight of bureaucratic tasks and administrative duties also factor into job dissatisfaction and increased workloads, leaving those on the frontline depleted and unfulfilled.
Burnout and turnover peaked during the pandemic, but never fully went away. According to Mercer’s most recent report, 100,000 RNs left the workforce by 2022 due to stress, burnout, and retirement. They further suggest that as recently as 2023, half of all doctors and nurses still felt compelled to leave their roles in the next 2 to 3 years.
On a positive note, the AHA’s 2025 Workforce Scan highlighted that burnout and turnover dropped for the first time since the pandemic, but cautioned that these factors continue to exacerbate shortages.
5. Financial Challenges
Rising costs are adding to the strain of healthcare workforce shortages. With tighter budgets, organizations are struggling to invest in recruitment and retention efforts, relying on expensive temporary staffing to fill gaps. This not only drives up costs but often leads to compromised care and inefficiencies.
To stay competitive, healthcare systems must offer higher pay and more benefits, but this can create a financial burden. As the cycle continues—higher staffing costs, increased turnover—organizations find themselves caught in a tough spot. Addressing these financial pressures is key to stabilizing the workforce and ensuring quality care.
Current Shortage Data & Statistics: Numbers Behind the Crisis
What does the data say about the state of shortages? Well, it’s not always so straightforward, which is why we’re gathering recently published sources to sift through the narrative. Figures and projections are constantly shifting and sometimes even conflicting with each other, so we’re examining the latest data to get a clearer picture of the gap between what has been said before and what’s expected. We’ll focus on shortage data affecting two heavily impacted areas: physicians and nursing.
Physicians
The AHA and AAMC both published separate reports in 2021, predicting that the U.S. would face a physician shortage of 124,000 by 2034, with primary care and specialty roles being hit hardest. The AAMC projected a shortage of 17,800 to 48,000 in primary care alone. However, in March 2024, the AAMC revised their prediction, now estimating a physician shortage of up to 86,000 by 2036. A more recent assessment (November 2024) by the Health Resources and Services Administration (HRSA) projected a shortage of 187,130 across all physician specialties by 2037—quite a jump from the AAMC’s estimate.
The United States Bureau of Labor Statistics (U.S. BLS) reports a 4% job outlook for physicians and surgeons (about average), while physician assistants (PAs) are seeing a much faster growth rate of 28% through 2032. It further notes that physicians and surgeons will have 23,600 openings annually for the next decade, while PAs will have nearly half as many—12,900. This suggests a potential expansion in the PA profession, and less growth for physicians and surgeons.
While these reports seem to indicate persistent and severe shortages, interestingly, Mercer’s 2024 analysis challenges the severity of physician shortages and even suggest surpluses. They do caution that shortages will vary between specialists and primary care roles, and that in certain regions skills gaps will persist.
Nursing
Nursing has been one of the hardest-hit sectors when it comes to workforce shortages, with demand outpacing all other health professions—especially throughout the pandemic. In fact, Epic Health Research found that hospital nurse staffing demands increased 245% (50,000 nurses) nationwide between September 2020 to December 2020.
Since 2019, the nursing workforce has increased 4.6% (including registered nurses, LPNs, nurse practitioners, nurse anesthetists, and nurse midwives). However, this increase has struggled to keep pace with the growing demand for nursing services.
What does the U.S. BLS say about the state of nurse workforce growth? Its Employment Projections for 2023 through 2033 anticipate job growth from 3.3 million in 2023 to almost 3.5 million in 2033. This translates to just 197,200 professionals entering the field over the next decade. The BLS further indicates that there will be 194,500 job openings per year for registered nurses. This means the total growth of 197,200 for the next decade will barely cover the need for one year (194,500).
Additionally, the US Chamber of Commerce expects 42 states to face nursing shortages in the next five years.
On the flip side, nurse practitioners (NPs), nurse anesthetists, and nurse midwives are thriving. These roles will see much higher job growth (40%) with fewer job openings (31,900) over the next decade. NPs are particularly noteworthy as they experienced incredible growth of 35.5% in 2023.
Nursing Assistants
Nursing assistant (NA) shortages are of severe concern, as highlighted in Mercer’s 2024 Report, especially considering that NAs make up a large portion of the healthcare workforce. Their research indicates a deficit of 73,000 nursing assistants by 2028. U.S. BLS data seems to support this considerable gap, estimating workforce growth for nursing assistants and orderlies will increase from 1.4 million in 2023 to 1.5 million in 2033—a minor growth of 64,700 over the decade. With an estimated 216,200 job openings each year, 64,700 won’t be sufficient to cover even one year’s demand.
Change of Perspective: Positive Projections
While several sources and studies point to enduring shortages in healthcare, a 2024 analysis by Mercer offers a different perspective. Like other reports, they acknowledge an impending shortage on the horizon but on a much smaller scale-- 100,000 healthcare workers by 2028 to be exact. They also anticipate growth in areas thought to face severe job deficits, such as physicians and nursing. Let’s explore some of their findings.
- Overall critical shortages of approximately 100,000 workers by 2028 (they emphasize it won’t be a crisis, but it will add continued strain)
- Shortages will vary by region and demographics, with some areas experiencing surpluses and others facing skills gaps
- A surplus of 30,000 registered nurses (with regional disparities)
- A moderate surplus of physicians at a national level (with regional disparities)

A Geographic Look at Workforce Shortages
When considering the magnitude of shortages, it’s important to recognize that they aren’t only about the number of workers. They also encompass regional and specialization gaps. What does that mean? While workforce projections may estimate a positive inflow of healthcare workers overall, shortages will persist in certain regions, particularly rural areas, and across specific specialties, such as primary care physicians and nursing assistants.
Rural areas are especially vulnerable to shortages and limited resources, forcing several to reduce or even close services. This is detrimental to communities in need of essential services, particularly when considering that roughly 75 million people live in a primary care Health Professional Shortage Area (HPSA). In its survey of over 6200 hospitals and 400 health systems across the nation, the AHA identified that 2/3 (65%) of community hospitals are in urban areas, while rural counterparts make up 35%.
Geographical Disparities
Though Mercer’s report predicted surplus trends of physicians and nurses by 2028, they project regional disparities for specific specializations. Here’s a breakdown:
Regional General Worker Shortages: While states like California, Texas and Pennsylvania aren’t expected to face general workforce shortages, states such as New York (61,473), New Jersey (17,769), Tennessee (-16,719), Massachusetts (-12,329) and Georgia (-11,308) will experience significant understaffing. New York in particular is expected to experience the most severe deficits. Refer to Figure 1 for detailed numbers and comparisons across specializations and states.
Regional Physician Shortages: By 2028, physician shortages will be most critical in New York (-2,706), Texas (-2,830), California (-2,580), Georgia (-850), and Missouri (-634). While California and Texas have a positive overall outlook, physicians remain a vulnerable point.
For current state shortage data, check out this helpful map by Rural Health Information Hub.
Registered Nurses: Mercer’s projections indicate a surplus of 30,000 registered nurses by 2028, although this contrasts with the U.S. BLS’ outlook. Despite the surplus, Mercer identifies regional shortages in New York (-12K), Massachusetts (-4K), Tennessee (-3K), New Jersey (-3K), and Kentucky (-2K). The US Chamber of Commerce has a different take on nurse shortages by region and predicts that by 2030, 42 out of 50 states will experience nursing shortages with North Dakota, Colorado, Texas, Florida and Nevada experiencing pronounced nursing gaps.
Nursing Assistants: Both the U.S. BLS and Mercer data agree on the upcoming shortages in nursing assistants, which will be harmful if left unaddressed. Regional shortages include California (-14k), Texas (-12k), New York (-11k), Florida (-4k), and New Jersey (-4k).
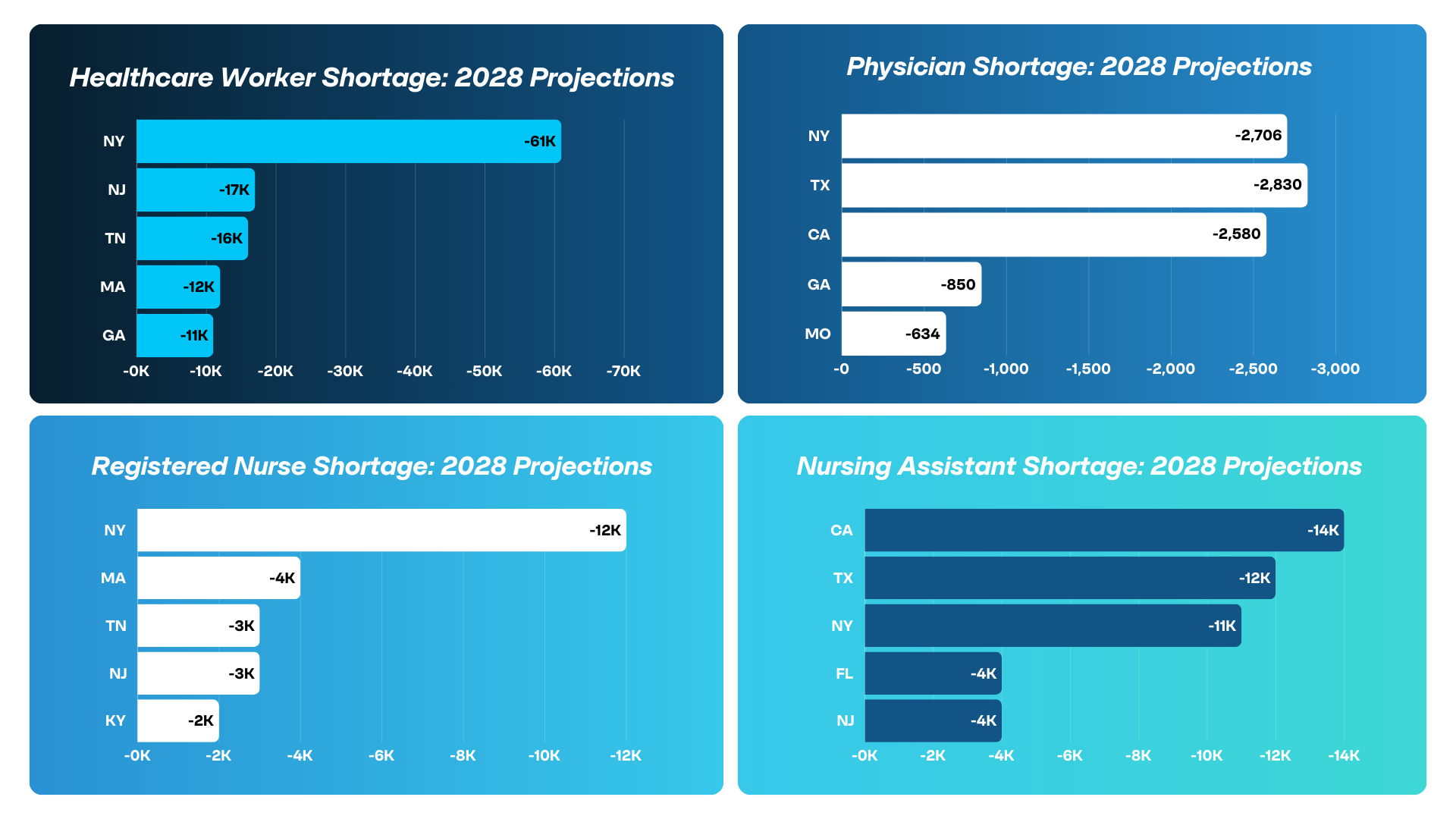
It's interesting to note that Mercer's report identifies heavily populated states like New York, California, and Texas as being greatly affected by shortages. However, it's unclear whether their numbers reflect urban or rural areas within these states.
Impacts of Workforce Shortages
We’ve explored the scope of workforce shortages—what they are, their causes, and the data behind them. Now, let’s dive into their significance. These shortages have profound effects on patients, employees and healthcare organizations. From increasing patient times to exhausting an already strained workforce, it's critical to understand their detrimental effects.
Patient Impact
Patient care suffers greatly from workforce shortages, resulting in longer wait times, reduced access to care, and compromised quality. For example, one study recently found that the average wait time for the third next available appointment is now 38 days, far exceeding the unofficial industry benchmark of 14 days. These delays can worsen patient outcomes, prolonging diagnoses and treatment or allowing conditions to progress unchecked.
Labor gaps also force facilities to close or limit the services they offer, impacting vulnerable populations such as low-income individuals, immigrants and those in rural areas. Reduced access to services often makes it difficult for people to receive the care they need and worsens health disparities.
Several studies continuously confirm the correlation between understaffing and negative healthcare outcomes. Research by the Columbia University School of Nursing revealed that nurse understaffing increases the risk of health care associated infections (HAIs). Another analysis highlighted how overworked clinicians, lacking adequate support, often rely on safety workarounds to meet demands, which raises the likelihood of near misses (potential accidents or injuries). Alarmingly, one study even suggests that in surgical settings, increasing a nurse’s workload by one patient is associated with a 16% increase in patient mortality risk.
Employee Impact
We’ve discussed how burnout has fueled shortages, but it’s equally important to consider how shortages, in turn, fuel burnout. Insufficient staffing places greater demands on already overworked employees, leaving them physically, emotionally, and mentally exhausted. With heavier workloads and diminished work-life balance, job dissatisfaction rises, workplace morale drops, and turnover becomes more likely.
Additional factors, like the emotional toll of compromised patient care, the burden of administrative tasks over direct patient interaction, and limited access to support, worsen the issue. Burnout reached new heights during the pandemic, but it continues to be a pressing issue. Tackling this challenge is essential for fostering a healthier workforce, strengthening retention, and drawing in future talent.
Organizational Impact
Workforce shortages take a serious toll on health organizations, making it harder to operate smoothly and efficiently. Teams often find themselves stretched too thin, leading to longer wait times, overworked staff, and reduced access to care for patients. On top of that, the financial pressure can be immense as organizations turn to expensive temporary staffing just to keep things running.
Lastly, brand reputation can suffer—when quality slips or patient experiences decline, trust deteriorates within the community, and potential employees may hesitate to join.
Solutions to Address Healthcare Workforce Shortages
Addressing workforce shortages requires a balance of human-centered approaches and technological innovation. These shortages impact real lives—from patients to our employees—so we need strategies that support our workforce where they are. By investing in employees' well-being, reducing their burdens, and restoring joy in their work, we can build a healthier, more sustainable environment.
At the same time, technological advancements and partnerships with educational institutions and workforce experts are key to securing future talent and ensuring long-term workforce sustainability.
The following solutions can make a significant impact:
- Immediate tactical solutions for short-term relief
- Recruitment and retention strategies
- Long-Term talent development and education
- Embracing technology to address shortages
- Strategic partnerships for a long-term workforce
- Policy and systemic approaches
- Shifting care delivery models
- Promoting public health & preventative care
1. Immediate Tactical Solutions:
Short-term relief for urgent staffing needs is sometimes necessary, leading many to turn to temporary staffing. True, this method can be costly, and its overuse has contributed to unsustainable workforce practices. However, external staff can provide valuable support when used strategically and in healthy amounts. Remember not to rely on this method as the sole solution to address shortages. Instead, it should serve as flexible support while working toward a long-term, financially sustainable solution to resolve workforce challenges.
Key short-term solutions include:
- Expanding Talent: Use traveling clinicians, per diem staff, and international hires to fill gaps during peak demand.
- Virtual Nursing: Adopt telehealth and remote nursing to quickly expand capacity and ease staff workloads.
- Temporary Staffing Solutions: Partner with staffing agencies or implement flexible contracts to onboard temporary staff quickly.
- Retired or Former Staff: Re-engage retired or former employees temporarily to leverage their experience and fill urgent gaps.
- Cross-Training Existing Staff: Cross-train current employees to take on additional roles, minimizing the need for external hires.
2. Recruitment and Retention
Attracting top talent requires staying competitive in a market where clinicians can work anywhere. A strong Employee Value Proposition is essential. This should include competitive compensation, benefits, career advancement opportunities, a positive culture, and a welcoming, diverse community. Just as important as attracting talent is retaining the workforce you already have. Many initiatives that draw new employees also ensure current team members feel valued, fostering loyalty and long-term commitment.
- Competitive Compensation & Benefits: Equitable pay, flexible benefits, sign-on bonuses, and role-specific perks help reduce turnover and attract top talent.
- Career Advancement & Work Culture: Clear career pathways, skill development programs, and an inclusive culture promote job satisfaction and a sense of purpose.
- Well-being Initiatives: Stress management programs, mental health support, and work-life balance initiatives prevent burnout and demonstrate care for employees.
- Employee Feedback & Recognition: Regularly seek input through surveys and group discussions, involve staff in decision-making, and implement recognition programs to celebrate achievements, boosting engagement and morale.
- Building Community: A culture of teamwork, respect, and open communication strengthens relationships, creating an environment where employees want to stay.
- Diversity, Equity, & Inclusion: Committing to DEI fosters a respectful, empowered workforce, enhancing satisfaction and retention while attracting diverse talent.
3. Long-Term Talent Development and Education
Building a sustainable workforce pipeline is essential amidst projected staffing gaps and rising costs. Engaging with talent early and investing in the development of current employees ensures preparedness for future challenges. Many organizations are forming educational partnerships to connect with future professionals, fostering familiarity and relationships that pay off over time.
- Partnerships with Academic Institutions: Collaborate with universities, trade schools, and community colleges to create career pathways through internships, co-ops, and mentorship programs.
- Upskilling and Reskilling Programs: Internal training and certifications help retain employees, close skill gaps, and adapt the workforce to evolving needs.
- Ongoing Education: Support continuous learning with online courses, micro-credentials, and leadership development programs to prepare employees for advanced roles.
4. Embracing Technology
Healthcare staffing challenges are complex, but technology is transforming how we manage them. From simplifying recruitment to making care delivery more efficient, the right tools can lighten the load and create lasting solutions. Whether it’s improving shift management or enabling virtual care, here’s how tech is stepping in to make a real difference:
- AI in Recruitment: AI-powered technologies, like vendor management systems (VMS), streamline processes such as resume screening, candidate matching, and interview scheduling, reducing time-to-hire and allowing recruiters to focus on high-value activities.
- Data & Predictive Analytics: By leveraging both real-time insights and historical data, analytics tools help healthcare organizations adjust staffing levels dynamically and forecast future needs, minimizing gaps and shortages.
- Scheduling & Flexibility Apps: Emerging solutions (like our StaffBot Flex app!) empower employees to manage shifts and request time off, enhancing work-life balance, retention, and overall satisfaction. Want to know more? Reach out to us here!
- Telehealth & Virtual Care: Telehealth expands capacity by enabling remote consultations, reducing on-site demands, and optimizing resource use.
- Remote Patient Monitoring (RPM): RPM solutions allow clinicians to monitor patients remotely, reducing in-person visits and enabling staff to focus on critical care.
5. Strategic Partnerships for a Long-Term Workforce
Creating a sustainable workforce model is essential in the coming years to overcome staffing challenges and financial pressures. Strategic partnerships with organizations that specialize in building talent pipelines and utilizing technology can be key investments in securing a future-proof workforce.
- Permanent Labor Workforce Solutions: Implement RPO (Recruitment Process Outsourcing), Float Pools, and Direct Placement programs to efficiently manage both short-term staffing crises and long-term workforce stability.
- Internal Staffing Agencies: Build internal staffing models to increase recruitment flexibility and reduce reliance on external agencies, enabling a quicker response to changing staffing demands.
- Data-Backed Workforce Consulting: Use data-backed workforce consulting to design tailored staffing strategies, improving operational efficiency, cost management, and more.
- Collaborations with External Providers: Partner with external workforce organizations to broaden the recruitment pipeline, fill staffing gaps faster, and build a stable, long-term workforce.
6. Policy and Systemic Approaches
Addressing workforce shortages requires not just operational changes, but also advocating for systemic reforms. By engaging in policy discussions and advocating for broader changes, healthcare organizations can help shape a sustainable workforce for the future.
- Policy & Advocacy: Collaborate with policymakers to address systemic issues like wage stagnation, credentialing barriers, and broader access to healthcare.
- Healthcare Workers’ Voices in Legislation: Advocate for including healthcare workers in policy development to ensure their needs and professional growth are considered.
7. Shifting Care Delivery Models
Adapting care delivery models is a key measure in addressing shortages and improving efficiency. Here’s how shifting responsibilities and expanding care settings can make a difference:
- Addressing Physician Shortages: Shift responsibilities to nurse practitioners and physician assistants, particularly in primary care, to alleviate pressure on physicians.
- Expanding Home-Based and Community Care: Promote home care and community partnerships to manage the aging population, reduce hospital readmissions, and provide cost-effective care.
8. Promoting Public Health & Preventative Care
Prioritizing public health and preventative care is essential in reducing future workforce burdens. By focusing on proactive measures, healthcare organizations can help keep populations healthier and lessen the strain on resources. Here's how:
Prioritize Preventative Care: Focus on education, resources, and public health initiatives to help people stay healthy, reducing the demand for medical services and easing workforce strain.
Conclusion
While healthcare workforce shortages continue to challenge us, there’s reason to be hopeful. Although certain regions and specialties will still face gaps, we’re seeing signs of growth and balance in the industry. By embracing technology, putting people first, and focusing on smart strategies, we can overcome these challenges. Together, we can innovate and prioritize the wellbeing of our workforce to ensure high-quality care for everyone.
We’re Here to Help You Solve Your Workforce Challenges
Hey there, we’re Staffency! We’re here to help empower organizations by creating workforce strategies for long-term success. Through collaboration and creative thinking, we build tailored solutions that solve specific challenges.
At the heart of our approach? A combination of technology, data-driven insights, and the human touch. This balance has led to 100% client retention for over 10 years.
Our offerings include:
- VMS Technologies: VMS solutions that streamline recruitment, automate compliance, enhance data-driven decision-making, and support those building internal staffing programs.
- Flex Pool and IRP Apps: A self-scheduling app that seamlessly manages your float pools, enhancing cost control, efficiency, and promoting a better work-life balance for employees.
- Permanent Workforce Solutions: RPO programs, direct placements, and float pool solutions to help build your team.
- MSP Services: We manage all or part of your external workforce to meet both immediate and long-term staffing needs
Curious about what might be best for your workforce challenges or have any questions? Let’s talk! Book a no-obligation consultation with us!
This blog is also featured as an article in our LinkedIn Newsletter. Join us there to share your thoughts and insights!